 Indexed in Index Medicus and Medline
Indexed in Index Medicus and Medline
Legends in Urology

Warren T. Snodgrass, MD PARC Urology
Dallas, Texas, USA
Editor’s Note: What Dr. Snodgrass modestly calls the Tubularized Incised Plate
(TIP) repair, urologists learned as the ‘Snodgrass Repair ’.
Many surgeons have asked me what it’s like to have an operation named after me. That was never a goal. Rather, tubularized incised plate (TIP) occurred by a serendipitous observation, and the task of defining its use and limitations became the focus of my career. For this article I was invited to describe the development of TIP, and the evolution of my practice from general urology to general pediatric urology to hypospadiology.
Hypospadias repair was so confusing to me as a junior urology resident! Dr. David Gibbons, a new faculty surgeon at Texas Children’s Hospital, began each case carefully studying the anatomy and then sketching his impressions and options for repair on the surgical drapes – a process that easily consumed up to 30 minutes and a handful of marking pens, and left me totally bewildered. It was 1982, one year after Dr. John Duckett published the meatoplasty and glanuloplasty (MAGPI), and Gibbons, his former fellow, along with Dr. Edmond Gonzales were trying to better determine its indications and contraindications.
The most frequent repair done by Dr. Gonzales was the Mathieu flip-flap, and one feature of that technique was the potential difficulty passing a catheter after the neourethra was made, as it seemed inevitably attracted to the small pockets created by the flap on either side of the original meatus. So Dr. Gonzales taught us to insert the catheter before flipping the flap to avoid that annoyance. I wrote down this key step, and others of the techniques I learned, on 4 x 6 index cards to use when I started my own practice.
Nearing graduation, Dr. Gonzales suggested I do a pediatric urology fellowship, which, in the mid-1980s, most often led to an academic career. But Dr. Gene Carlton had organized one of the first subspecialized residency programs at Baylor, and after learning cancer surgery from Dr. Peter Scardino, stone surgery with Dr. Don Griffith, infertility from Dr. Larry Lipshultz, and prosthetics with Dr. Brantley Scott, I was eager to apply all their lessons. Besides, an academic post meant doing research, and I could not think of anything I wanted to study.
I’m sure my decision to become a urologist in the first place was influenced by the fact that my father was a urologist. As residency ended I considered a few job offers, and then decided to join him in Lubbock doing general urology.
The sparse population there generated only a handful of new hypospadias repairs each year, but I was well-trained, and confident that with those index cards, I could choose the best operation for the anatomy and then perform it as I had been taught.
Consequently, I was both disappointed and disconcerted when my first patients returned after Mathieu repairs with a round, unsightly neomeatus. Residents did not attend faculty clinic during my training, and so I had learned the technique, but not its result. I discussed my concern with former fellows I trained alongside, and one summarized their collective response that “if the opening is on the glans, and there are no complications, then it’s a success. You can’t expect to make something abnormal look normal.”
Failure opens the mind to new considerations, and after reading Dr. Mark Rich’s paper describing urethral plate hinging to make round openings vertical, I resolved to try it on the next patient. After cutting the skin flap for a Mathieu, I next incised the plate as Rich advised, from the midglans distally, and noticed how widely it expanded. I decided to continue incising more proximally, eventually into the meatus, and realized the urethral plate was now so wide that the flap was not needed. I passed the catheter and tubularized the plate over it, covered the neourethra with a dartos flap, and then finished the glansplasty.
Afterwards I looked through old urology textbooks, including a first edition Campbell’s, in my father ’s library, curious what operation I had done. In an era before the internet I could not find a similar procedure in his collection, or in various articles the hospital librarian tracked down for me. In 1992, I presented preliminary results to the South Central Section, knowing that Dr. Terry Allen, an associate editor for the Journal of Urology, would attend. If this technique was the old operation resurrected, he would know. But he said nothing.
It took a full 3 years to accumulate the 16 patients that comprised the first reported cohort. I wondered why Duckett (or others) did not make the same observation while hinging the plate. I eventually learned that he made the neourethra over a larger catheter which he exchanged for a smaller one, and at that point slipped in a 15 scalpel blade to blindly hinge the plate. The incision I made a few steps earlier under direct vision is the reason I was invited to write this recollection.
The new operation needed a title, in keeping with the times that produced “MAGPI”, “GAP”, and “Transverse Island”. I devoted some effort to this project before deciding on “TIP” (tubularized incised plate), which captured both the key step and the final result. After the first paper was published in 1994, Dr. Martin Koyle gathered results from some of the earliest converts – Dr. Richard Ehrlich, Dr. Tony Caldamone, Dr. Rick Hurwitz and Dr. Tony Manzoni – and invited me to present our combined data to the AAP. I needed help with slides, and called Koyle’s office. He was out, and when his secretary asked who was calling, immediately responded, “Dr. Snodgrass? THE DR. SNODGRASS?”
You might imagine that having a name like Snodgrass resulted in some ridicule as a child. How ironic that others decided this would be the name of the procedure! Nevertheless, I have never called it anything other than TIP.
I have since learned how conservative surgeons are, how reluctant many, possibly most, are to make changes in what they do. Yet this operation spread from Lubbock like a prairie grass fire around the world to become the most commonly used technique for distal hypospadias repair. After a hypospadias podium session a few years later, my comoderator Dr. Bill Cromie casually asked the audience how many used TIP? When it appeared nearly everyone raised their hand, he leaned over and said to me, “Maybe never in history has an operation been so rapidly accepted. I thought you should see this.”
Although MAGPI, Mathieu, GAP and other procedures then used for distal repairs all were described in publications as giving excellent cosmetic results, clearly surgeons realized TIP was conceptually straightforward and reliably created a normal appearing penis.
The first proximal TIP was in 1993, on a boy with proximal shaft hypospadias that I planned to repair with an onlay flap. After degloving, I was concerned that the subcoronal urethral plate was narrow and might stricture. My private nurse assistant suggested I just incise it, as I did distal repairs, and the wide enlargement that resulted showed again that a flap was not needed.
When I saw that I wanted a picture, but my camera was at the office. I called my secretary, and then waited until she arrived, carefully folding the plate back together to look untouched. This photograph became an illustration in the first proximal TIP report.
The small volume of cases in Lubbock meant I could not define the role for TIP without moving to a larger city. But initial offers to relocate to Philadelphia or Dallas fell through because I was not fellowship trained. Then one Sunday morning Dr. Mike Mitchell, whose junior colleague was moving, called to offer a 1 year position, providing him with experienced help, and me with credentials.
I had no desire to become a division chief, but 2 years after I arrived in Dallas, Dr. John McConnell made the proverbial offer that left me no room to refuse. Still new to academics, I had no idea how to proceed, so I arranged breakfast with Dr. Alan Retik and then followed his advice to build a program that grew into a fellowship training center.
Dallas is a long afternoon drive from Lubbock, and I knew that some of my patients would follow me there. So I took the paper charts from my former practice with me, only to realize they did not fit into the Children’s record system. Soon they were laying around the office trying to get lost.
A key milestone in my career was extracting pertinent information from those charts before they were misplaced, following Dr. Doug Husmann’s example when he moved from Dallas to the Mayo Clinic years before. I entered these data into an Excel spreadsheet, then realized I had done 82 hypospadias repairs in my 12 years in Lubbock and 1 year in Seattle, and could immediately see their follow up and complications. I resolved to keep adding the new hypospadias patients I managed to this database.
Because of this, I learned that I had complications in 53% of those initial proximal TIP patients, 33% being fistulas despite using a dartos coverage flap in every one. Dr Mitchell had watched one of these repairs, and suggested I do a two-layer subepithelial urethroplasty rather than the single layer epithelial closure I used - but at the time this seemed to me unnecessary. Once again, failure opened my mind to the need to improve, and I first changed the urethroplasty as he advised, then later the coverage flap to tunica vaginalis, and documented a significant reduction in complications with no fistulas in the last cohort.
This was the first example of the 3 Ps, Prospective data collection, Periodic outcomes review, and Practice changes to improve – an early form of evidence-based surgical practice. This experience prompted me to begin other personal quality databases regarding neurogenic bladder, nonpalpable testes, and Deflux injection, among others. The consistent lesson was that my results in everything I reviewed were never as good as I thought, yet got better after I realized the need to change.
But those Excel spreadsheets had limitations. Dr. Nicol Bush laboriously dummy-coded the more than 1000 hypospadias cases in that database 8 years later so that SAS could better analyze the data. Now, in addition to simple determinations of case volume and results, logistic regression could be applied to understand the factors influencing those outcomes.
I struggled for years to learn how to best correct proximal hypospadias when the urethral plate needed to be transected during penile straightening. I quickly gave up on the transverse island and turned next to Byars flaps, but 100% of my patients developed complications! Then I changed from these prepucial flaps to staged prepucial grafts, with a 50% reduction in complications. Logistic regression showed the impact that the small glans in many of these patients exerted, and Dr. Bush additionally found that enlarging it with preoperative testosterone did not reduce related complications.
A fortuitous visit to Japan in 2012 - to observe a graft technique used by Dr. Saburo Tanekazi and Dr. Kaoru Yoshino - showed me a better way to dissect the glans wings for glansplasty and reduce glans dehiscence. With this modification, Dr Bush and I now correct the most severe cases of hypospadias with 80% initial success, which increases to nearly 100% after one, or rarely two, distal reoperations.
But we had been discussing glans dehiscence for many years - presenting abstracts at international congresses, publishing peer-reviewed articles in prominent journals, showing videos at the AUA – yet, when we described our new glansplasty several surgeons told us they always did it that way! I even noticed a figure in an old Duckett article that showed more extensive glans wings dissection than I was taught, but wasn’t emphasized as a key technical step.
Meanwhile, a colleague recently mentioned that if there are 30 surgeons there are 30 different ways to do a TIP repair. Unfortunately, that is a true reflection of years of surgeons telling themselves their personal experience is the most important determinant of their results, “doing what works for you”. But there are not 30 ways to do a TIP that all give the best possible outcomes, and another lesson I have learned is that no surgeon knows his or her experience until they have actually tallied their results.
Many recent publications show there is room for improvement in hypospadias surgery, one national European study reporting complications ranging as high as 63% in boys after distal hypospadias repair. But even the best published results show that approximately 1 of every 10 boys undergoing distal repair will need at least one additional operation for complications, as do many more after proximal repairs.
Having come into pediatric urology for hypospadias, and then expanding my interests to investigate a broad swatch of the specialty, I now end my career focused, almost exclusively, on hypospadiology. Dr. Bush and I established PARC Urology in 2014 specifically to improve care for boys with proximal hypospadias, and men with the residual effects of hypospadias repair gone wrong.
There are only 1,000 boys born each year in the United States with proximal hypospadias, and logs submitted to the American Board of Urology show that the median number of these repairs done annually by certified pediatric urologists is only 2. Clearly, that is not sufficient volume to gain, and then maintain, expertise in correcting the most severe forms of this affliction of the penis. Dr. Bush and I are following the example of other centers managing complex conditions - working together as an experienced, and data-driven, surgical team in all these operations.
By simplifying the algorithm, hypospadias repair is no longer confusing. By continuously monitoring our results, we ensure we are doing the key steps optimally. By focusing on hypospadias surgery rather than general pediatric urology, we have a large volume to maintain our expertise. By working together as a surgical team, we bring two sets of experienced hands to each operation. By choosing my successor, I have assured that the lessons I have learned are not forgotten, but continue as a foundation for future improvement.
Having experienced the limitations of traditional academic teaching and learning we are resuming live-surgery webinars, knowing that surgeons benefit from watching other surgeons operate. We even offer individualized webinars to those who refer us a difficult case so that they can participate remotely in the procedure.
After publishing a textbook summarizing the evidence available for decision-making in pediatric urology and discovering that the publisher keeps all the profits from our labor, Dr. Bush and I self-published a textbook last year, Hypospadiology, and are using all proceeds to fund Operation Happenis, a non-profit to raise public awareness about this birth defect. Perhaps our cash-strapped societies could similarly self-publish our journals and textbooks and use the profits to fund education and research.
Having shared my experience applying the 3 Ps with surgeons worldwide, repeating that message year after year in meeting after meeting, I now learn that handfuls have adopted this practice pattern too. Their stories are uniformly the same – when they reviewed their results they were not as good as they thought, which challenged them to improve. But every day children are still harmed by well-intentioned surgeons who have not realized there is a better way to care for them, which starts with knowing your own results.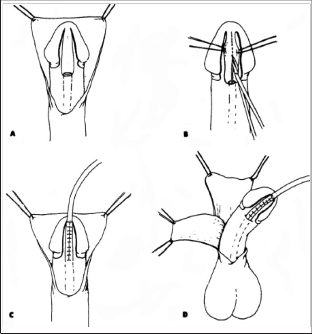
We all need mentors to help lay the foundation for our careers, but the house we build in practice needs constant renovation. I warned each fellow at graduation to not go out to do things the “Snodgrass way” they learned, since that would likely not be the way I would be doing things in a few years when I reviewed my latest results!
Warren T. Snodgrass, MD PARC Urology
Dallas, Texas, USA
Figure from the 1st TIP report. Note that the urethral plate is shown tubularized too far distally in “c”, which can result in meatal stenosis!
8787
© The Canadian Journal of Urology™; 24(3); June 2017

